Recent research has shone a light on fascial dysfunction as a source of pain or injury in
track & field and other sports. In the second half of this article, Editor Russ Ebbets
asks the author specific questions to clarity the subject matter.
By Emmet J. Hughes, D.C., M.S.
Fascia is a component of the connective tissue made up of sheets of collagen and elastic fibers that are associated with loose connective tissue. This loose connective tissue allows normal gliding of the individual layers of collagenous and elastic sheets that make up the deep fascia. It is a continuous, three-dimensional supportive structure found throughout the body, enveloping every blood vessel, nerve, muscle, bone, and organ. It is richly populated with sensory receptors providing a continuous feedback mechanism to the central nervous system. It is crucial for local coordination of groups of muscles, allowing them to act synergistically to enact movement.1
There are three main types of fascia found in the body: superficial, deep (which includes both aponeurotic and epimysial fascia), and visceral fascia.
Superficial fascia is found deep in the superficial adipose tissue (SAT) just below the dermis. It is firmly adhered to the skin via vertical septa (retinaculum cutis superficialis) interposed between the SAT. It is also connected via diagonal septa (retinaculum cutis profundus) found in the deep adipose tissue (DAT) layer to the deeper fascial layers known as aponeurotic fascia and epimysial fascia.
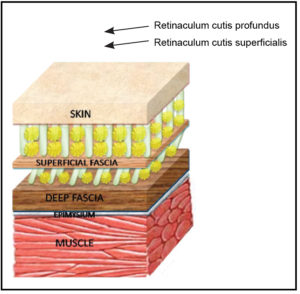 Epimysial fascia consists of two to three layers of fibrous sheets, mainly collagen fibers with some elastic fibers, with layers of areolar connective tissue in between each sheet. Previously, the arrangement of the collagen fibers was thought to be disorganized. Recent studies demonstrate that the arrangement in each layer is quite organized along specific lines of stress.2 Each sheet is oriented in a different direction giving the tissue the appearance of disorganization, thus the descriptive term dense, irregular connective tissue.
Epimysial fascia consists of two to three layers of fibrous sheets, mainly collagen fibers with some elastic fibers, with layers of areolar connective tissue in between each sheet. Previously, the arrangement of the collagen fibers was thought to be disorganized. Recent studies demonstrate that the arrangement in each layer is quite organized along specific lines of stress.2 Each sheet is oriented in a different direction giving the tissue the appearance of disorganization, thus the descriptive term dense, irregular connective tissue.
The hyaluronan between each sheet acts as a lubricant, allowing the layers to glide over one another. Changes in pH, inflammation and direct trauma can cause the hyaluronan to polymerize, entangling the molecules and changing the consistency from a lubricant to more like honey or glue. These areas have been termed densifications. This can be a significant source of pain and dysfunction.3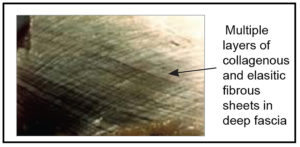
Without the normal gliding of the fascial sheets, dysafferentation from proprioceptors in the fascia cause a discoordination of the muscle groups controlling the joint they are associated with. On average, 47% of the muscle fibers are not continuous with the tendon, but rather are invested in fascia. These fibers tense the fascia causing mechanical stress and firing of mechanoreceptors. Abnormal stresses in the fascia due to changes in the hyaluronan can lead to abnormal movement and joint damage.
To restore normal glide to fascia, a practitioner must be able to identify the specific points in the fascia where the densifications occur. A thorough history of traumas suffered over the patient’s lifetime is essential in honing in on where the densifications may be that are causing the current symptoms. Treatment involves manual deep friction over the densifications to restore normal gliding. This can be achieved using knuckles or elbows.
Patients who suffer from insidious pain syndromes and chronic pain should be evaluated for fascial dysfunction. By restoring the normal function of the fascia, the normal proprioception is restored and allows for proper coordination of movement. Many of these patients can function optimally and with minimal or no pain after years of suffering with chronic pain and dysfunction.
- Benjamin M. The fascia of the limbs and back−a review. J Anat. 2009 Jan;214(1):1-18.
- Klingler W, Velders M, Hoppe K, Pedro M, Schleip R. Clinical relevance of fascial tissue and dysfunctions. Curr Pain Headache Rep. 2014;18(8):439.
- Pavan PG, Stecco A, Stern R, Stecco C. Painful connections: densification versus fibrosis of fascia. Curr Pain Headache Rep. 2014;18(8):441.
- Stecco A, Stern R, Fantoni I, De Caro R, Stecco C. Fascial Disorders: Implications for Treatment. PM R. 2016 Feb;8(2):161-8.
1. What is the fascia? Fascia is a dense “irregular” connective tissue that forms a 3-D structure, enveloping muscles, nerves, blood vessels, lymphatics and organs.
2. How has our understanding changed about the fascia in the last 20 years? Fascia was previously thought to be inert. We now know that fascia acts as a sensory organ and has contractile elements.
3. How would one know if they have a “fascia problem” as opposed to a muscle tear or chronic tendonitis? A fascial problem is generally recognized as different from a strain or sprain in that there is an insidious onset, usually to an area of the body that hasn’t had trauma. Chronic tendonitis (tendonopathy) can be due to fascial dysfunction. The history of the patient would be another clue as to whether or not it is a fascial problem.
4. Warren Mattes said the fascia is one of the water storage areas of the body…has this understanding changed? It is much more than a water storage area. Although the hyaluronan does imbibe water, I wouldn’t consider it a water storage area.
5. What do you see as the most common fascial injuries? How do they present? Chronic “trigger points”, compartmental syndromes, insidious neck and low back pain are common fascial problems. Often they will present with unexplained weakness in a muscle or group of muscles, without any neurological deficit.
6. Are the “densifications” you mentioned the same thing as adhesions? It depends on what an adhesion is described as. A densification is an increase in the density of hyaluronan, not an increase in collagen. That would be better described as a fibrosis. A densification fits the definition of an adhesion in my view.
7. How does a healthy fascial system aid one’s symmetry of motion? What about force and power production? A healthy fascial system is crucial to symmetry of motion. It allows proper recruitment of muscles to move a joint in a specific plane.
8. What type of health care practitioners do fascial work? How would one find someone in their locality? What questions should one ask? Rolfers, massage therapist, physical therapists and chiropractors do fascial work. However, looking at the fascia in a holistic way is different than the traditional therapist. It is an approach that requires extra training. In my experience, Fascial Manipulation (Stecco method) is superior in that it takes that holistic approach.
9. If the fascia is healthy how does it contribute to the stretch reflex? (I am thinking about the pronation/supination of the hands and feet that tighten the fascia and make it more spring like—is this a correct assumption?) It does contribute to the stretch reflex. The most recent research on this has turned our basic understanding of the physiology of muscle activation on its head. It is understood that the gamma motoneuron is first stimulated by descending pathways (corticospinal tract) and that activates the muscle spindle. The contraction of the muscle spindle activates the Ia afferents (spiral endings) which relay a signal to the cord activating the extrafusal fibers associated with that spindle. It acts as an “on” switch for the extrafusal fibers.
10. Who are some of the pioneers in the fascial work? Ida Rolfe, Meyers, Mattes, and Luigi Stecco are certainly the ones I think of. Carla and Antonio Stecco have done a lot to advance our more recent understanding of fascia.
11. How do their philosophies or approaches differ? I think that the Steccos have advanced treatment of fascia way beyond anyone before them. They bring the unique perspective of treating fascia from the point of view that old injuries affect the ability of the fascia to convey sensory information and that by restoring glide to the fascia, one restores the sensory function as well.
12. One of the common training maxims is to train “movements not (individual) muscles.” Why does this make sense as one understands the fascial plane? It is perfectly matched to the most recent research. I think it is quite ridiculous to think that we can train a single muscle. In my view, that is a primitive way to look at movement.
13. How can the fascia be injured? Changes in pH, trauma, chronic inflammation, overstressing are all ways to “injure” the fascia. This leads to densifications and fascial dysfunction.
14. Is there any way to “strengthen” the fascia? I’m thinking here of isometric-type exercises, other movements, nutrition, etc. Certainly movement in specific patterns (i.e. plyometrics) help to maintain the function of fascia. I’m not sure that increasing the density of the collagenous structure would be a good thing for the fascia.
15. What effect does traditional static stretching have on the fascia? It has a beneficial effect. However, as far as I know, it will not resolve densifications.
16. How do disciplines such as Tai Chi and yoga affect the fascia? What about disciplines like Feldenkrais Method and Alexander Technique that actors use? These are all great to maintain the function of the fascia, but will not address densifications.
17. Track & field has a high incidence of hamstring injuries and Achilles injuries—how could the fascia be involved with these areas? I believe that underlying densifications are a causative factor in these injuries, as well as other injuries.
18. How does the fascia affect posture or conversely how does posture affect the fascia? Densifications in fascia will negatively affect posture and vice versa. Poor posture can lead to the development of densifications.
19. How does one’s warm-up affect the fascia? What about a warm-down? I think that warm-up is more important in preventing injuries. Post-exercise stretching is an excellent way to maintain the proper function of fascia.
20. Should one think of “loosening up” the fascia or is it more an elastic tissue that responds better to range of motion type exercises (or something else)? In my experience, deep cross-friction massage over densifications is what does the trick. This is the only way that I know of that a manual medicine practitioner is able to restore the glide in fascia. I know that there are some successes using injections of hyalruonidase (an enzyme that breaks down hyaluronan).
21. There are many tools on the market that purport to treat the fascia—are there any you recommend more than others? (foam rollers, Tiger Tal, etc.) Without the knowledge of how the fascial system works, these are limited in their value. Looking at agonists and their antagonists is a critical way to restore the gliding to the fascial system.
22. If you look into your crystal ball—what changes do you see with regards to care of this tissue in the next 10-15 years? I was just at a “master class” in Arizona. We were training the Arizona Diamondbacks manual medicine team (athletic trainers, strength coaches and massage therapists) in this technique. I think it will become a staple of all professional sports teams. I believe that this is a revolution in the way fascia is looked at and treated.
23. Are there any You Tube videos that you feel are valuable or would recommend? I haven’t seen many that are that helpful. I did see a woman from Finland who works with children who suffered brain injuries. She had some amazing videos of dramatic improvements in the ability of these kids to ambulate after being treated using Fascial Manipulation.
24. Anything else you’d like to add? I encourage manual medicine practitioners to learn the technique. I encourage coaches and teams to seek out someone who is adept at doing this technique. This will help to keep your athletes competing instead of nursing chronic injuries.
Emmett J. Hughes, D.C., M.S. earned his doctor of chiropractic degree from the University of Bridgeport College of Chiropractic in 1997. He is an Associate Professor of Basic and Clinical Sciences at UBCC and has been teaching there for 20 years. He has published numerous articles on nutrition, basic science, and fascia and continues to do research in those areas. He maintains a private practice in Huntington, NY.